In this interview, Timothy Noakes, Ph.D., a physician and sports medicine researcher in South Africa, clarifies common confusions about sports hydration and high-carb diets.
Noakes graduated from medical school in Cape Town, South Africa, in 1974, and received his research degree a few years later. Since then, he’s published more than 750 papers and a number of books, including the groundbreaking, “Waterlogged: The Serious Problem of Overhydration in Endurance Sports.”
“Waterlogged” countered the conventional view that you should drink as much as you can, even before you feel thirsty, to optimize your hydration. As it turns out, that can be dangerous advice for endurance athletes.
Overhydration Can Be Deadly
In early 1981, Noakes wrote an article arguing that runners must drink as much as they possibly can tolerate when running. “I’d been pushing that story for about 10 years,” he says.
A few months later, he received a letter from a woman who’d competed in the Comrades Marathon, a 56-mile South African ultramarathon. Some 40 miles into the race, she started losing her cognitive faculties and her husband took her to a medical facility.
Doctors declared that she was dehydrated and gave her 2 liters of intravenous normal saline (0.9% NaCl), at which point she lost consciousness and had an epileptic seizure. Her blood sodium was 112 units, well below the normal 140. Had she been given more dilute saline at this point, she may have died. Fortunately, the attending doctor restricted fluids and just waited. It took four days for her to regain consciousness.
“She’d been told she’d lost a lot of salt … and that this was the problem. I said to her, ‘Well, I have no idea, because this is the first case ever reported.’ But obviously, I was interested to find out [more]. So, I started phoning around and studying it.
Turned out there was another athlete who’d suffered a similar problem in the same race. And then I found another two cases. So, by 1985, I had four cases and it was clear to me that all had drunk too much fluid during the race …
The reason is because as the blood sodium concentration drops, the fluid expands the brain, and so the brain volume starts to increase. Ultimately, the pressure rises, stopping the blood flowing in or flowing out. As a consequence, the part of the brain that controls breathing herniates through the base of skull, and then you stop breathing. So that’s the cause of death. You stop breathing.”
According to Noakes, the treatment for overhydration is to give a high-saline IV (3% to 5% NaCl). Your kidneys cannot hold that much sodium, so it’s released into your urine where it helps expel the excess water through urination. Basically, the sodium acts as a diuretic. People usually make a rapid recovery within minutes to hours with this treatment.
Why Some Are Prone to Dangerous Overhydration
Because of all this, Noakes reversed his position on hydration during marathons, and published a paper on the dangers of fluid overload in 1985. Alas, the sports drinks industry in the U.S. was taking off at that time, and American runners were told to drink as much as possible, so his advice was not well-received.
“I predicted that the first person who would die from this condition would be a female runner in an American race,” Noakes says, “and that’s exactly what happened. In 1993, a runner in a California marathon died after the race. And again, she finished the race, she was semi-conscious, and then she was treated and the treatment was wrong.
Ultimately, we were able to prove that the condition doesn’t occur in everyone who overdrinks. Most people who overdrink simply pass more urine … What happens in this condition is that they’ve got inappropriate hormone secretion, antidiuretic hormone, and they retain fluid even though they’re overhydrated …
I think it’s genetic, in the sense that you either have it or you don’t. I think about 10% to 20% of people have that condition, so that when they overdrink, the body doesn’t recognize it as being overhydrated. It still thinks it’s dehydrated …
They’re running along and not passing urine, so they think, ‘My gosh, I’m dehydrated, so I must drink more.’ And that fluid is retained because this hormone is so powerful at retaining water. Ultimately, the brain swells and they lose consciousness.
Provided you leave them alone or give them a solid high-sodium infusion, they’re fine, but if you give them a low-sodium infusion, you’re going to kill them. I was demonized for saying all this. Eventually I wrote ‘Waterlogged,’ which … describes the whole history of what happened and [why] you should just drink to thirst.”
Prosecuted for Breaking With Dietary Convention
Noakes also broke with conventional nutritional advice when he started recommending a high-fat diet. One day, he read a book called “The New Atkins for the New You,” and realized his dietary advice was likely completely wrong.
He decided to try the Atkins diet, which is a high-fat, high-protein, low-carb diet, and “had spectacular results,” including reversing his Type 2 diabetes. He recounts what happened next.
“I joined Twitter and did this very famous tweet [about the benefits of a low-carb diet] which caused me to be charged by the medical profession in South Africa for unprofessional behavior.
I had to go to court for over four years. Eventually I won the case and proved that the low carbohydrate diet has plenty of evidence behind it. It’s not unscientific. It’s in fact the most scientifically studied diet in the world.
So I won that case … At the same time, I was asked to start helping some other people with research and we started delving deeper, doing studies that I hadn’t done before on low carbohydrate diets.
Essentially, we are on the cusp of proving that humans don’t need carbohydrates … but when you come from an athletic background, you can’t believe that. Well, we’ve taken it to the extreme and we’ve shown that athletes who eat a high-fat diet, their performance is perfect, it’s completely normal.
So, my opinion is that the dietary macronutrient composition — the amount of carbohydrate and amount of fat you’re eating — has no effect on your athletic performance with one exception.
But the reason you burn carbohydrate is very clear to me. You burn carbohydrates to regulate your blood glucose concentration. That’s the key element of metabolism — to regulate your blood glucose.”
It is interesting that as a long-distance runner, Noakes developed diabetes. I used to believe that cardio was the cure for diabetes. It is well-known now that this is simply not the case. Food choices are responsible for causing diabetes.
However, excess carbs and not enough fat are not the reason someone develops diabetes. It is interesting to note that in 1890, about 2.8 people per 100,000 had diabetes. Today that number is likely north of 30,000 if you include those with prediabetes. That is a more than 100,000 times increase in a little over 130 years.
Increases in sugar intake or carbs did not cause this. It was the introduction of seed oils that caused severe mitochondrial dysfunction, causing the body to burn fatty acids rather than glucose. While limiting carbs can help when one develops diabetes, the solution is to radically reduce seed oils and every milligram of processed foods.
Athletes Don’t Need Carbs, Research Shows
Noakes believes humans didn’t have the need to regulate blood glucose until more recently, because we evolved eating mostly high-fat, high-protein diets. “We didn’t have a need to regulate blood glucose concentration because we weren’t eating stuff that was raising it,” he says.
I have great respect for Noakes and he is a kind and wonderful human being, but I believe that he is seriously mistaken on this point. He is just as confused as I was a few years ago on this issue. While fats can clearly fuel endurance cardio participants, that is entirely different from understanding what the best and most optimal fuel is for the mitochondria.
Noakes believes that over the last 50 years or so, we started eating very large quantities of carbs, but because our biology isn’t designed to cope with all those carbs, the coping mechanism is to burn it as soon as it’s consumed to lower the blood glucose level.
Sadly, the data simply don’t support Noakes’ assertion. From 1935 to 2016, the percentage of calories from sugar in the American diet rose only marginally from 22.5% to 24%. That’s an increase of just 1.5 percentage points.
Meanwhile, the consumption of seed oil skyrocketed from around 7% of total calories, which is still three times the recommended daily allowance (RDA), to a staggering 29% — nearly one-third of the modern American diet. So, while sugar edged up slightly, seed oils experienced exponential growth over the same time. Noakes continues:
“That’s why, when we study athletes who are eating a high carbohydrate diet … you see they’re burning so much carbohydrate, but they’re burning it to get rid of it, not because they need to use it,” Noakes says.
“We are the first people in 100 years to show that fat-adapted athletes can burn fat at very high rates in high intensity exercise, to the point where you could run a two-hour marathon burning fat alone. That’s what the data suggests.
We haven’t had a person run a two-hour marathon on a high fat diet, but the amount of energy required by Elliot Kipchoge when he runs a sub-two-hour marathon, is about 80 kilojoules per minute. Fat can provide 76 kilojoules per minute at least.
So he could run that race just burning fat, which of course conflicts with everything we’re taught. So that’s where we’re at, at the moment, and I’m working vigorously on finalizing the documents which prove that humans don’t need carbohydrates for exercise.
They can do very well with a minimum amount of carbohydrate … all you need is just to maintain your blood glucose concentration. Your blood glucose concentration is under stress during exercise, because even if you’re fully fat adapted, you can’t quite generate enough glucose to maintain your blood glucose for more than about three or four hours.
So, ultimately, if you don’t have carbs and if you’re a low-carb athlete, after about four hours you run into trouble. We are testing that hypothesis. We want to determine the minimum amount of carbohydrates you need, much as we determine the minimum amount of fluids you need during exercise.”
Processed Food Is a Primary Driver of Ill Health
I also embraced low-carb early on, and wrote a best-selling book called “Fat for Fuel.” So, I really understand the concept. I’ve endorsed it and recommended it. And, while my current recommendations have changed somewhat, I still think there’s great value in low-carb, primarily because most Americans are metabolically inflexible and insulin resistant. If that applies to you, a low-carb diet can help you regain your metabolic flexibility.
That said, since I wrote “Fat for Fuel,” I’ve come across additional information that has forced me to reconsider the value of staying on a low-carb, high-fat diet long-term. The late Ray Peat, a pioneer of bioenergetic medicine, advocated a relatively high glucose diet, but with specific types or carbs.
It is important to have carbs that have fructose in them, as fructose is an important fuel with many beneficial effects if it is consumed in the form of whole foods. The best foods with fructose are fruits and honey. Conversely, starches are long polymers of glucose with virtually no fructose.
Starches like white rice and white or red potatoes can be safely consumed if well-cooked, but most other starches are not digested in your small intestine, but travel to your large intestine where they are digested and form endotoxin, which is highly problematic for your health.
Curiously, evidence suggests both low-fat, high-carb, and high-fat, low-carb diets work equally well for Type 2 diabetes, but this would be extraordinary extremes, as health blogger Denise Minger points out in a lecture I plan to post soon.
I suspect the reason for that is because both diets tend to be whole food-based, so it’s really the avoidance of processed food that makes the biggest difference, and the single most destructive ingredient in processed food, based on my current understanding, is the omega-6 fat linoleic acid (LA).
So, to be clear, what Noakes is finding is that you don’t need carbohydrates to compete effectively in endurance events. I think that’s probably true, but the reason I went into medicine was because I have a passion to be healthy and to live as long as I can and teach others how to do that. And for a healthy life span, I now believe that optimizing glucose metabolism in your mitochondria is the key.
Glucose Appears To Be an Optimal Fuel for Health
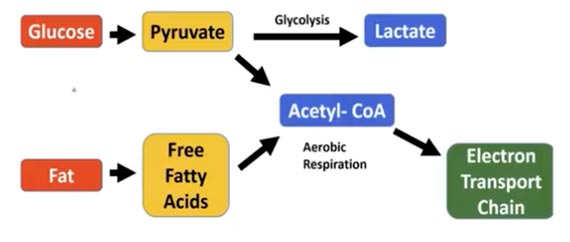
Up until recently, I was convinced that fat was the ideal fuel to burn as a substrate in your mitochondria, but Peat’s work suggests that’s not true. What’s more, while you could technically survive without carbohydrates, because your body can make glucose from other substrates, that comes at a significant price.
The supposition is that to optimize longevity, you must optimize mitochondrial efficiency, and to do that, you want to burn the fuel that creates the most ATP and the least amount of ROS. If you have forward electron flow in the mitochondria, you can get to 99.9% efficiency.
Reductive stress facilitates reversal electron flow in the mitochondria, which raises ROS generation 30 to 40 times, and one of the things that contributes to reductive stress is beta oxidation of fat.
When beta oxidation occurs, the electrons don’t jump to Complex 1 in the electron transport chain; they jump to Complex 2, which contributes to reductive stress. And, while LA is the worst culprit, causing the greatest amount of reductive stress, even healthy saturated fats will have this effect.
In addition to creating far less ROS, burning glucose in your mitochondria will also generate far more carbon dioxide and metabolic water, as opposed to creating lactate when it is burned in glycolysis.
What’s more, when your glucose level gets too low, you’re going to secrete cortisol. Cortisol creates glucose by stripping amino acids from your bones, brain and muscles. So, the danger of going low-carb long-term is that you can end up with chronically elevated cortisol, which leads to a lot of complications, including sarcopenia (muscle loss).
I believe Noakes’ observation may be related to the fact he was working with cardiac cells, which are an exception to most tissues in your body, as at rest, heart cells are designed to burn fat, not sugar. Noakes comments:
“The focus for my Ph.D. was, what was the fuel that made the heart perform the best? And I came to the conclusion that glucose and insulin were actually the optimum, but the very first experiment I did was to add ketones to glucose and the heart functioned a lot better.
I left it at that and didn’t deal with it any further, unfortunately, because Richard Veech did exactly the same experiments 10 years or so later, and came to the conclusion that ketone metabolism was crucial for whole body metabolism.
If I read the introduction to his article, therapeutic potentials of mild ketosis flow directly from a thorough understanding of their metabolic effects, particularly upon mitochondrial redox states, energetics and substrate availability …
There’s a lovely book, ‘Ketones, the Fourth Fuel,’ written by Travis Christofferson, in which he talks about [Otto] Warburg … Hans Krebs [and] Veech … They were the three people who really promoted ketone metabolism and its understanding.
So I’m not the authority, but it seems to me that ketones do have a special role in mitochondrial metabolism, and do exactly what you’re suggesting the carbohydrates do …
Veech came up to the conclusion that ketones had a special role in minimizing mitochondrial electron overflow, as you suggested, and oxidative stress. But I haven’t really studied closely enough all his research …”
How Much Fat Is Too Much?
An expert in the Randle cycle, Noakes agrees that high amounts of fat inhibit glucose metabolism, which is why you cannot simply add more carbs if you’re eating high amounts of fat. Your body simply won’t be able to burn those extra carbs for fuel.
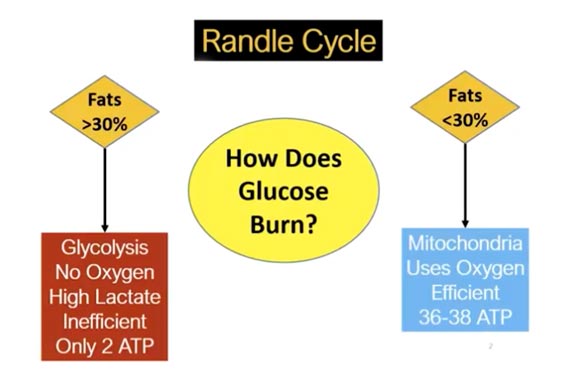
The Randle cycle is going to inhibit the oxidation of glucose in the mitochondria, resulting in weight gain, reduced energy production and other problems. If you’re metabolically impaired, as most people are, your fat intake may need to be as low as 10% to 15% initially, to prevent glycolysis from occurring.
Over time, you can then raise your fat intake to about 30% and still maintain healthy glucose metabolism. Unless you minimize your LA intake and get your total fat content below 30%, you really can’t go high-carb, because the end result is predictable. It’ll lead to diabetes, especially you have high tissue levels of LA, because the glucose cannot be metabolized in your mitochondria and will go to glycolysis instead.
You also cannot load in just any type of carbohydrates. Most grains are loaded with LA and are therefore best avoided. Resistant starches also need to be limited, as they fuel the production of endotoxins in your gut.
The best carbs are ripe fruits. In addition to being a source of carbohydrates, ripe fruits also contain high levels of potassium, which will balance your sodium. Other healthy carbs include white rice and well-cooked potatoes.
Noakes’ Model: Muscle Glycogen Determines Fat Metabolism
Interestingly, in 1999, Noakes did a study showing that it’s not the Randle cycle that determines fat metabolism but, rather, the muscle glycogen content. In other words, the amount of glycogen in your muscles determines how much fat you burn. He explains:
“We made people glycogen depleted, and then we infused glucose. The glucose infusion made no difference. They refused to burn the extra glucose because they were burning so much fat when the glycogen was low.
In fact, I found an old paper [showing] that the best way to normalize your glucose tolerance is to get your muscle glycogen to zero, or as low as possible, and that fits my model.
My model is that when you take carbohydrate, the first thing you do is you try to burn it, so you inhibit fat oxidation, and then you dump it into muscle … and then you’ve got to exercise, get rid of it, and you cannot stop muscle glycogen burning. You cannot.
You can do what you like, it doesn’t stop muscle glycogen use. So, you can infuse glucose at high rates, the muscles will still burn the glycogen. If there’s glycogen in the muscle, it will be burned. And you have to ask why, when there’s so much fat to be oxidized?
So that’s the model that I see. I see the human as being loving to burn fat, and we’ve destroyed that by feeding them linoleic acid and carbs for too long. That’s how I see it.”
Why Strength Training Is so Important
Importantly, muscle glycogen is only used in the muscle. The glycogen cannot be excreted or secreted into your bloodstream. Only glycogen in the liver can do that. This makes a strong case for resistance training and building significant muscle mass. Like me, Noakes switched from running to doing resistance training when he got older:
“I’ve also shifted to weights and resistance training and it’s astonishing. When I look back, the benefits I get as a 74-year-old from resistance training are equal to the benefits I used to get at running as a 20 year old or a 30 year old. Today I can’t get those benefits from running anymore.
You have to change. And I’ve met a lot of endurance athletes who’ve told me that once they crossed 60, they reduced the running or the cycling and moved into resistance training, with huge benefits.”
Life Requires Constant Adaptation
In conclusion, Noakes correctly (and humbly) admits that when it comes to diet and exercise, we cannot make absolute statements that will be correct and always apply to everyone. We have an obligation to experiment and discover what works best for us, in the moment, and realize that what was best a few years ago may no longer be ideal.
To give you a personal example, when I shifted over from high-fat, low-carb to relatively high-carb, low-fat (upping my carbs from 150 grams a day to 400 or 500 grams) I lost 10 pounds, my body fat decreased 3% and my fasting blood sugar went down 10 points.
So, my body was telling me, “This is something I want to do.” It was clear that, from a blood work perspective and biological parameters, I was moving in the right direction. That intrigued me, because I like to test these theories out on myself before I start espousing them to others.
Before that, I was convinced that long-term high fat, low carb dieting was the way to go. My experience told me I hadn’t completely nailed it and needed to refine my recommendations further, which is why I’m now presenting more information about the benefits of higher-carb, lower-fat diets.
The caveat is that you need to be mindful of the types of carbs you add in, and to avoid seed oils. Unless you lower the LA, high-carb is not going to be a good strategy. Also, if you’re not exercising enough, eating 500 grams of carbs is going to be a disaster.
To learn more about Noakes’ work, please visit thenoakesfoundation.org. Also consider sponsoring his research efforts by making a donation, or become a research participant by filling out an anecdotal data collection form.

