In the midst of the coronavirus pandemic, two certainties emerge in the lives of physicians: they are generating less revenue, and they have adopted more virtual care in practices.
 The Physicians Foundation surveyed 3,513 physicians in July 2020 on their perspectives on COVID-19 and how the pandemic has impacted practices and patients. This study is part one of three conducted by the Foundation this year, subtitled the “COVID-19 Impact Edition” of the 2020 Survey of America’s Physicians which the Foundation conducts each year.
The Physicians Foundation surveyed 3,513 physicians in July 2020 on their perspectives on COVID-19 and how the pandemic has impacted practices and patients. This study is part one of three conducted by the Foundation this year, subtitled the “COVID-19 Impact Edition” of the 2020 Survey of America’s Physicians which the Foundation conducts each year.
Merritt Hawkins conducted the study on behalf of the Foundation, shifting the focus to the pandemic. This post in Health Populi covers the first of 3 parts, on patient impacts. Part 2 will cover the impact of COVID-19 on physician well-being, and Part 3, on the impact of the coronavirus on the health care system.
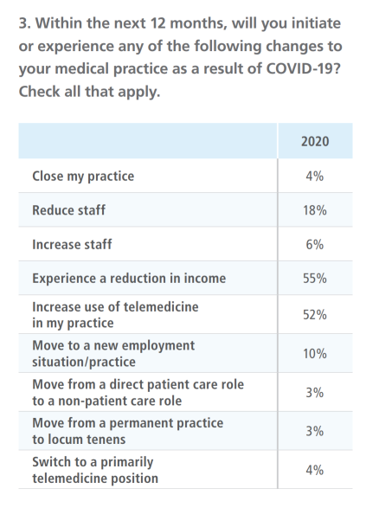
One-half of physicians in the U.S. believe the pandemic won’t be under control until sometime after June 1, 2021. Eight percent of doctors have closed their practices as a result of COVID-19, tallying about 16,000 closed practices. Another 4% expects they would close their practice in the next 12 months, shown in the first table.
The two impacts impact most physicians as a result of COVID-19 have been experiencing a reduction in income (55%) and increasing the use of telemedicine in the practice (52%).
4 in 10 doctors saw patient volumes fall by at least 26%, which the Foundations noted could be difficult or impossible for most physician practices to sustain for more than a few months.
Because a plethora of patients have postponed seeking medical care from their doctors, 43% of physicians have reduced staff; another 18% expect to do so in the next year, the chart also indicates.
Due to patients delaying care, three-quarters of doctors are concerned that COVID-19 will have serious consequences for patient health in their communities.
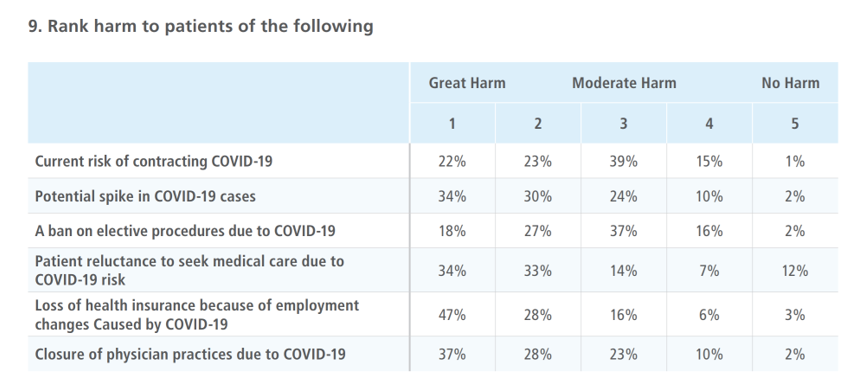 Interestingly, when considering various factors that could cause great harm to patients, the current risk of contracting COVID-19 ranks lower than other concerns.
Interestingly, when considering various factors that could cause great harm to patients, the current risk of contracting COVID-19 ranks lower than other concerns.
Ranking top for great or high harm, three in four physicians said that the, “loss of health insurance because of employment changes caused by COVID-19” would cause great harm to patients.
Two-thirds of doctors are also concerned about closure of practices due to COVID-19 causing great harm to patients.
Most physicians are also worried about harm done to patients by postponing medical care: two-thirds of doctors rank this as great harm, along with 64% of doctors concerned about a potential spike in COVID-19 cases.
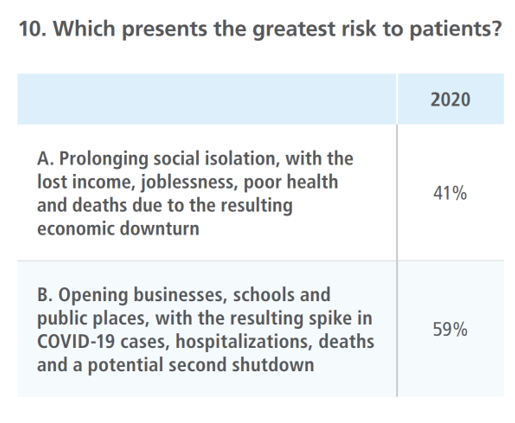 The third table here exhibits physicians’ response to an (A) or (B), either-or question on what presents greatest risks to patients: prolonging social isolation, with lost income, joblessness, poor health and deaths due to the economic downturn; or, opening business, schools and public places resulting in a spike of COVID-19 cases, hospitalizations, mortality and potential second shutdown?
The third table here exhibits physicians’ response to an (A) or (B), either-or question on what presents greatest risks to patients: prolonging social isolation, with lost income, joblessness, poor health and deaths due to the economic downturn; or, opening business, schools and public places resulting in a spike of COVID-19 cases, hospitalizations, mortality and potential second shutdown?
Most physicians point to (B), opening the economy “too soon” before the spread of the coronavirus would be under control.
This is the short- versus long-term economic argument of “when” to open up.
Counterbalancing the lack of in-person visits, thousands of physicians have pivoted to virtual care and telemedicine platforms. Twelve percent of doctors told the Foundation they had moved to a primarily telemedicine practice due to the pandemic, a “sea change in how physicians deliver care,” the Foundation asserted in its report.
They estimate that the number of physicians now seeing patients through telemedicine is 15 times greater than the number two years ago.
One-half of doctors plan to increase their use of telemedicine in the next 12 months, the survey learned, across both primary care and specialty practices.
85% of doctors believe the use of telehealth will become much more widespread after the pandemic, with the majority of physicians cautioning that telemedicine’s persistence will depend on both parity for payment and lowering of administrative burdens.
Still, 73% of physicians said they should work as a profession to ensure telemedicine remains widely available to patients, essential to providing patient care.
 Health Populi’s Hot Points: The physicians have spoken: most believe telemedicine should be health care delivery as one channel of several for providing patient care, in and after the pandemic abates.
Health Populi’s Hot Points: The physicians have spoken: most believe telemedicine should be health care delivery as one channel of several for providing patient care, in and after the pandemic abates.
That’s the supply side of the market speaking, with demand on both patient and payor fronts also coming forward in the pandemic to support virtual care.
A survey published by Metova last week featured survey results of over 1,000 U.S. consumers, conducted in August 2020. Four in five consumers would choose telemedicine for their next medical appointment, with 79% wanting to connect with a medical professional using video conferencing and 93% satisfied with the experience.
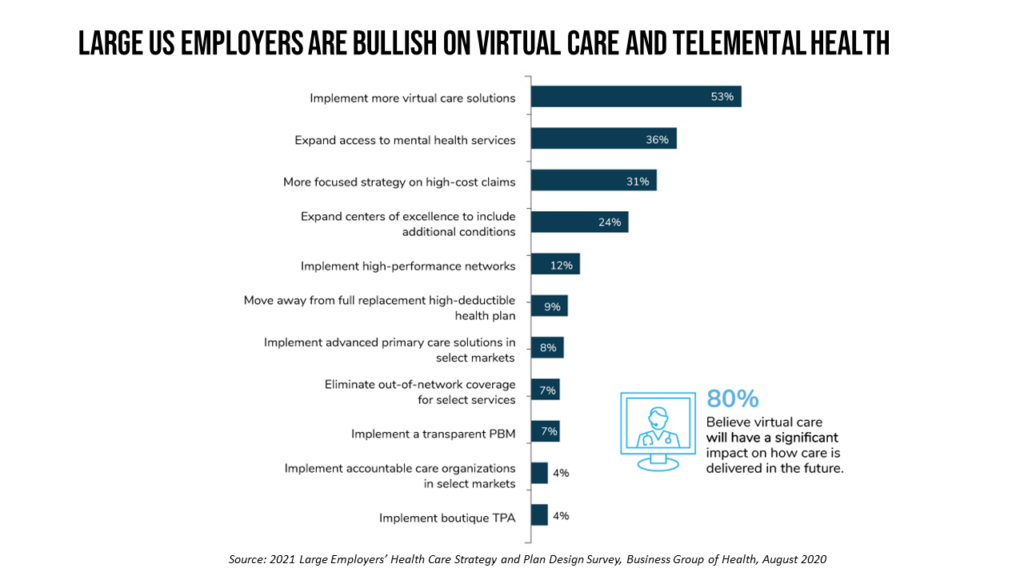
On the payor front, large U.S. employers are accelerating their adoption of virtual care for both medical and mental health services, based on the 2021 Large Employers’ Health Care Strategy and Plan Design Survey from the Business Group of Health. Four in five large employers believe virtual health will play a significant role in how care is delivered int he future, up from 64% in 2019 and 52% in 2018.
Furthermore, nine in ten companies plans to offer virtual care for telemental health, a fast-growing aspect of virtual care. Employers are looking to expand emotional well=-being support, with worker demand in the pandemic an epidemic growing out of the pandemic.
That’s the private sector bullish approach to telehealth after the pandemic. We await to see how the public sector — namely Medicare and the Centers for Medicare and Medicaid Services — will respond for payment and administrative policies post-COVID-19.
