Introduction
The pharmaceutical business model requires pharmaceuticals that are “effective” enough to somehow justify pushing them on patients but not effective enough to actually fix the issue the drug is prescribed for, thus requiring each patient to take the drug indefinitely. Furthermore, the larger the potential drug market is, the more aggressively the pharmaceutical industry will push to promote it to every available customer.
In some cases, such as for the dangerous and ineffective COVID-19 vaccines, this greed is so blatant even the general public can see it. Conversely, in other cases, it is typically invisible to any besides those directly affected by the drugs and their immediate family.
Recently, for example, I reviewed the statin catastrophe after Aseem Malhotra on the Joe Rogan show brought the public’s attention to the danger and ineffectiveness of these drugs and how the same reprehensible forces we saw push the COVID-19 vaccines have been operating for decades within the cholesterol industry.
Although it’s challenging to claim any one class of drugs is the “worst,” a good case can be made for psychiatric medications. In addition to the drugs being dangerously addictive and most of their “benefits” coming from doctored research data, they have some disturbing side effects.
Beyond already tragic complications like fatal heart attacks (which happened to a close friend of mine), individuals on these drugs can become partially psychotic, and there are many tragic cases of suicides and homicides following their use.
Unfortunately, because of just how large this market is, the industry and the FDA have gone to extreme lengths to cover up the harms of these drugs for decades, and business as usual continues in the psychiatric sector.
Note: Much of this is difficult to believe, so I chronicled exactly what can now be proven happened with the antidepressants. I did this because what the FDA did back then is one of the closest precedents we have for understanding how the COVID-19 vaccines were handled and what to expect will happen in the future.
After I published an article summarizing the evidence for the psychotic, violent, and often deadly behaviors these drugs caused, Kim Witczak reached out to me to share her story. Soon after Zoloft entered the market, Kim’s husband Woody was unnecessarily put on the drug and, not long after, suddenly killed himself in a manner characteristic of a Zoloft suicide.
Kim decided the best thing she could do with this tragic situation was to work to prevent it from happening to anyone else. She had numerous successes and was instrumental in a black box warning for suicides being placed on SSRI antidepressants (something she believes would have been impossible to accomplish in today’s much more corrupt political climate).
Due to her work, Kim became the consumer representative on the FDA’s Psychopharmacologic Drugs Advisory Committee and is frequently the only dissenting vote on unjustifiable drug approvals.
Note: This is analogous to how Ron Paul earned the nickname Dr. No during his time in Congress because he was frequently one of the only dissenting voices against unconstitutional legislation. Kim periodically shares distressing things she observes with me:
“I am going to write about it, but I was once again the only no vote. This meeting was about using the antipsychotic Rexulti for an “unmet” need of Alzheimer’s Agitation indication. The data was minimal, and yet the death analysis was double the antipsychotic rate that the FDA calculated from a meta-analysis of other antipsychotics.
Anyway, the committee voted 9-1 to recommend approval for the “unmet” need. The reality is that the government has been cracking down on [dangerous and difficult to justify] antipsychotic use in nursing homes.
They have noticed a rise of [likely fraudulent] schizophrenia diagnoses. So this will help the industry get their drugs covered [by insurance] and used in nursing homes. I told the FDA they need to watch the marketing and communication around this product to ensure the benefits are not overstated, and death downplayed.
It is so discouraging, and yet I know there are people like you that are out speaking the truth. But hey, at least I got the media to call me out for being the lone dissenting vote on this one!”
Note: A much more detailed summary on the absolute absurdity of this approval written by Kim can be viewed here. Recently, Kim shared something I believe has immense value for the entire public to know. However, to fully appreciate it, we must first take a quick detour into Alzheimer’s disease.
Alzheimer’s Research?
Alzheimer’s disease currently is one of the most devastating diseases in existence, both for the individual who experiences it (along with their family) and more broadly for society, as over 1% of global GDP is spent on caring for dementia (likewise in 2021 Alzheimer’s was estimated to cost the United States 355 billion dollars), and its cost has not stopped increasing.
Because of this, Alzheimer’s disease is a “national research priority,” and in 2021, 3.1 billion was allotted for Alzheimer’s and dementia research. Yet despite over a century of research (amyloid was first identified as the cause of Alzheimer’s in 1906), cures for Alzheimer’s remain elusive.
The conventional view of Alzheimer’s is that amyloid plaques, for some reason, accumulate in the brain and gradually destroy the brain as their concentration increases. Because of how aggressive the amyloid contingent has been, researchers exploring other Alzheimer’s models frequently refer to this contingent as the “Amyloid Mafia.”
Sadly, despite being studied for a century and often receiving billions of dollars in research funding each year (last year, 1.6 billion was allotted for amyloid research), the amyloid model has brought us no closer to treating the disease.
I originally wrote about this topic because an independent academic discovered that the data in a pivotal 2006 Nature paper (which “proved” the amyloid model and ended the growing dissent against it within the scientific community) had been fabricated.
Put differently, this meant that almost two decades of research (along with billions spent funding it) resulted from this fraud (e.g., one of its focuses which never received research support before 2006, received 287 million in research grants just for 2021).
Curiously, despite this fraud being investigated and confirmed by a premier scientific journal, the paper has not been retracted (there has just been a notice for the last year that it is being investigated). The lead author (Lensé) likewise has not suffered any consequences for his scientific misconduct (despite having since been found to have a much more extensive record of fraud in the many papers he’s published that “reconfirmed” his hypothesis). Instead:
“He [Lensé] became a leader of the University of Minnesota’s neuroscience graduate program in 2020, and in May 2022, 4 months after Schrag delivered his concerns to NIH, Lesné received a coveted R01 grant from the agency, with up to 5 years of support. The NIH program officer for the grant, Austin Yang — a co-author on the 2006 Nature paper — declined to comment.”
In short, there is immense corruption in this field of research. This, I believe, is a result of the pharmaceutical industry wanting to bury any research that threatens this cash cow (the scale of Alzhiemer’s makes it one of the most potentially profitable drug franchises in existence).
The scale of this corruption is possible because Fauci worked for decades to reshape the NIH to function as a pharmaceutical production pipeline where the NIH and its researchers are paid significant royalties for questionable pharmaceuticals they push through the approval process.
In the case of Alzheimer’s, this is particularly tragic because numerous viable treatments already exist for it — however, since they threaten the Alzheimer’s market, they have never been allowed to see the light of day.
What Causes Alzheimer’s Disease?
I know of a few methods that have shown promise in treating Alzheimer’s, yet sadly most researchers are unaware of them. All of my colleagues who have successfully treated the condition (or more commonly, slowed its progression) have arrived at similar conclusions on how to treat it (their approaches are discussed in more detail here):
Restore the blood flow to the brain. | Restore the lymphatic drainage from the brain. |
Avoid unnecessary toxin exposure (e.g., gas anesthesia is a common offender here). | Remove toxins from the brain (e.g., heavy metals with EDTA chelation). |
Provide essential nutrients to the brain (e.g., aluminum-free subcutaneous B1 and B12 shots). | Identify and treat chronic infections contributing to dementia (e.g., HHV6 or Lyme). |
Of these, the first two appear to be the most important and often require improving the zeta potential of the body. Additionally, I have one colleague who also utilizes stem cells in his regimen treating the condition, and while this does help, he emphasizes that stem cell therapy is unlikely to benefit the patient if the other areas listed above remain unaddressed.
Note: Conversely, the spike protein excels at triggering many of the causes of Alzheimer’s disease (e.g., it damages the blood circulation to the brain). One of the saddest complications of the COVID-19 vaccines has been their tendency to induce a rapid cognitive decline in the elderly (this, for instance, has happened to the parents of numerous friends). In each case, that decline is assumed to be a normal result of aging.
Likewise, I have seen many anecdotal examples of minor cognitive impairment following COVID-19 vaccination and more significant cognitive impairment in COVID-19 vaccine-injured patients and watched physicians present data showing this issue is widespread.
Since the successes of the above approaches utilized to treat Alzheimer’s are anecdotal, only used by a few practitioners, and have no clinical trials to support their efficacy, I can understand why the scientific community has not embraced or even tried to explore them. However, there is one integrative model for treating Alzheimer’s that has been proven to work in clinical trials, and yet despite this being the case, it too has been ghosted by the massive Alzheimer’s industry.
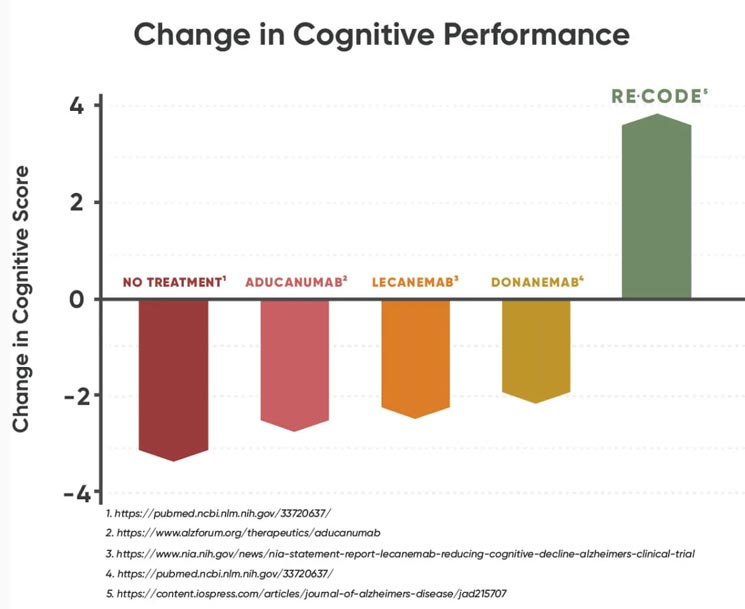
Note: In this trial, 84% improved, 12% declined, and 4% had no change in cognition from the RE-CODE protocol.
The brain always has processes that preserve neurons and processes that eliminate them (as this is necessary for the brain to adapt to the needs of the environment). Dale Bredesen, MD, in The End of Alzheimer’s, in turn, has made an excellent case that Alzheimer’s represents the destruction of neurons outpacing their creation and advocates for lifestyle practices and functional medicine interventions that reverse that balance so your neurons are protected.
The RE-CODE protocol was his attempt to do this, and unlike the approximately 400 failed studies which preceded it, this one actually worked.
Lead author Dr. Kat Toups noted, “I have been the Principal Investigator on more than 20 long-term clinical trials for patients with MCI and dementia where the benchmark for success was merely a slowing in cognitive decline. This trial is the first to show actual improvement in multiple domains of functioning, as well as improvements in MRI brain scans.”
One of the most critical points, Bredesen has made (I agree with) is that amyloid functions as a protective mechanism the brain utilizes against factors that would otherwise damage it. This means targeting amyloid, at best, is an exercise in futility and at worse, highly detrimental to the brain.
Amyloid Drugs
Given the scope of this problem and the continual failure of amyloid drugs (again, there are hundreds of failed clinical trials), it is quite surprising that Bredesen’s work has been completely ignored (although patients around the country seek out neurologists who Bredesen trained). Fortunately, at long last, the current FDA was able to find a solution to our inability to address the lack of a viable treatment for Alzheimer’s disease.
On June 17th, the FDA granted an accelerated approval for the first amyloid therapy. To quote their press release:
“This approval is significant in many ways. Aduhelm is the first novel therapy approved for Alzheimer’s disease since 2003. Perhaps more significantly, Aduhelm is the first treatment directed at the underlying pathophysiology of Alzheimer’s disease, the presence of amyloid beta plaques in the brain.
The clinical trials for Aduhelm were the first to show that a reduction in these plaques — a hallmark finding in the brain of patients with Alzheimer’s — is expected to lead to a reduction in the clinical decline of this devastating form of dementia.”
Note: I could not help but notice how much each of the FDA press releases I read for this article sounded like promotional material for the drugs written by the pharmaceutical industry.
The approval of Aduhelm was immensely controversial, to the point ten of the eleven members of the FDA panel voted against approving it (which is something not even the atrocious COVID-19 vaccines could achieve).
Three, in turn, resigned following the panel being ignored and Aduhelm nonetheless being approved, with one stating in their resignation letter that this was “probably the worst drug approval decision in recent U.S. history.” What, then could have accounted for the panel’s unprecedented rejection of a new lucrative product?
Simply put, Aduhelm failed to show any improvement for Alzheimer’s disease, while brain swelling or brain bleeding was found in 41% of patients enrolled in its studies.
More importantly, because the drug was priced at $ 56,000 a year (and therefore capable of bankrupting Medicare), this approval was followed by numerous calls for this approval to be investigated. Before long, a congressional committee convened for that purpose (which is highly unusual; even the COVID-19 vaccines have not met the bar for a formal congressional investigation).
Following an 18-month investigation, it found that serious irregularities occurred within the FDA’s approval process. For example, the agency sidelined its scientists who raised concerns about Aduhelm, and the FDA helped Biogen (Aduhelm’s manufacturer) prepare its presentation to the outside committee — something that has only happened nine times in the past (all for cancer drugs).
In short, while it was widely known that Biogen manufacturers and the FDA worked together on Aduhelm, to quote STAT News: “The back-channel relationship between the two started earlier and was far more extensive than disclosed.”
Similarly, because of the political backlash against the approval, the FDA was forced to conduct its own investigation, which, while less damaging than the congressional findings, identified similar issues and admitted the agency’s collaboration with Biogen “exceeded the norm in some respects.”
Additionally, one of the more interesting gems found within the congressional investigation was how Biogen planned to address the fact they were charging an exorbitant amount of money for an ineffective and extremely dangerous drug:
“Internal documents showed the company set “an unjustifiably high price” of $ 56,000 a year for Aduhelm because it wanted a history-making “blockbuster” to “establish Aduhelm as one of the top pharmaceutical launches of all time,” even though it knew the high price would burden Medicare and patients, the report found.
The investigation said Biogen was prepared to spend up to several billion dollars — more than two-and-a-half times what it spent developing the drug — on aggressive marketing to counter expected “pushback” over whether Aduhelm was worth its price [consider for a moment its cost, efficacy and safety].
The report said the campaign planned to target doctors, patients, advocacy groups, insurers, policymakers and communities of color, who were drastically underrepresented in its clinical trials of the drug.”
Note: Since this time, Biogen has halved the price for Amgen as many of its expected buyers decided the benefits did not justify its cost (likely due to the bad press the drug created).
Then on January 6, 2023, a second amyloid drug (with a slightly different target) was approved by the FDA, also produced by Biogen (this time in partnership with Eisai), and again was accompanied by a glowing press release from the agency.
Leqembi did a bit better than Amgen; only 21% experienced brain bleeding and swelling (compared to 9% in the placebo group), and 26.4% experienced infusion-related reactions. Conversely, there may have been a tiny benefit observed. When the 898 subjects with early-stage dementia who received Leqembi were compared to the 897 who received a placebo over 18 months, a small delay (27%) in cognitive decline was observed in those receiving the drug.
Furthermore, while this change was deemed to have reached statistical significance, the actual difference in symptoms between the treatment and placebo group in the trial was 0.45 points on an 18-point scale. To quote Medical Xpress:
“Most clinicians in the field suggest that a greater difference is needed to impact patients’ lives, for example 1 to 2 points.”
Based on how the data was collected, this small difference was likely an artifact rather than anything meaningful. Nonetheless, the field was overjoyed since, after decades of work, this was the first clinical trial ever to show a potential benefit for treating Alzheimer’s disease (a slight delay in its progression which nonetheless comes at a severe cost).
Responses like these help to illustrate the systemic blindness throughout the medical field given that Dale Bredesen already put forward a much cheaper, safer, and most importantly, dramatically more effective clinical trial that all of these researchers (who receive billions each year) are somehow unaware of.
The Revolving Door in Washington
One of the most important points RFK Jr. shared during his presidential campaign relates to his experience in spending decades litigating against federal agencies collaborating with corporate America in harming the American people. His observation was that the federal agencies were full of good people trying to do the right thing, but a corrupt leadership tied their hands.
This RFK Jr. argued was because our government structure favors unethical people who do not have America’s interests at heart ascending to the top of the bureaucracy (e.g., because corporate America lobbied for their promotion), and I fully agree with his assessment. Consider, for example, that the second official appointed by Trump to head the FDA (and helped pave the way for Operation Warp Speed), Commissioner Scott Gottlieb, is now on Pfizer’s board.
At the same time, the commissioner who was in charge of the FDA for the entirety of Operation Warp Speed, Stephen Hahn, is now a CEO-partner for the venture capital firm that launched (and owns) Moderna.
Sadly, bribing officials by promising them high-paying jobs after they leave office is not exclusive to medicine. Our current Secretary of Defense was initially a four-star general, then hired onto the board of Raytheon (a defense contractor), then appointed to his current position, and since he came to office, the most dangerous war in modern history has broken out, and Raytheon has made a lot of money.
To further support RFK Jr.’s argument, when the COVID-19 relief bills were passed, they contained a provision for the Government Accountability Organization (congress’s watchdog and one of the least corrupt agencies in the federal government) to investigate how the responsible federal agencies (the NIH, CDC, FDA, and ASPR) handled the pandemic.
This investigation (summarized here) found that employees in all four agencies observed political interference occurred, which prevented evidence-based scientific policies from being followed. Furthermore:
“Respondents from CDC and FDA told us they did not report potential political interference in scientific decision-making because:
- They feared retaliation.
- Being unsure how to report issues. Respondents from CDC and FDA stated they were not sure how to report the potential political interference in scientific decision-making they observed. For example, a CDC respondent told us they were not aware of any existing internal procedures that could be used to report potential political interference in scientific decision-making.
- Believing agency leaders were already aware. Respondents from CDC, FDA, and NIH stated they did not report potential political interference in scientific decision-making because they thought leadership was already aware of the issue.”
Note: This is also very similar to what members of the CDC have shared when attempting to draw attention to the significant corruption within their agency.
Furthermore, the GAO found that most of the policies that should have been in place to prevent this from happening (which were very simple and widely recognized as essential) were not:
“The absence of specific procedures may explain why the four selected agencies did not identify any formally reported internal allegations of potential political interference in scientific decision-making from 2010 through 2021.”
Furthermore, the GAO repeatedly observed officials argue that the lack of reported issues was proof those issues did not exist, and therefore meant nothing more needed to be done.
“Officials at CDC and FDA told us that there was not a specific reason why CDC and FDA lack such procedures and that the agencies did not intentionally omit this information [necessary for reporting fraud or violations of scientific integrity] from their existing policies and procedures.”
I hope that these examples help to illustrate how a significant number of FDA employees, for good reasons, could oppose Aduhelm’s approval — but nonetheless were overridden by the agencies leadership.
Note: Following the approval of Aduhelm and its successor, Billy Dunn, the Director of the Office of Neuroscience, Center for Drug Evaluation and Research (which was the division of the FDA responsible for approving these drugs) left the FDA and became a board member of a biotech company developing therapeutics for degenerative neurological conditions.
JP Morgan’s Healthcare Conference
When Kim contacted me, it was specifically about JP Morgan’s annual healthcare conference, a private invitation-only event described by JP Morgan as “the industry’s biggest gathering.” The 41st conference, from January 9-12, 2013, was the first one hosted in person since the pandemic started resumed being in person (it was hosted in San Francisco). Given this event’s impact on the year to come, Kim made a point to gleam as much as she could from its website.
Given what she found on public display, I can only imagine what was said behind closed doors. Since behind the scenes footage of the pharmaceutical industry is quite difficult to obtain, we only have a few examples to illustrate what actually transpires in this culture:
This circa 2000 clip of shows how Pharma sales reps are trained behind the scenes. Like Pfizer, GSK aggressively and illegally promotes drugs (like this one) and has received billions in fines.
I can’t even imagine how much wilder the industry has become since this was leaked. pic.twitter.com/gO1E1s2xfn
— A Midwestern Doctor (@MidwesternDoc) February 1, 2023
I now want to share some of the most important points Kim alerted me to. First, if you consider who was chosen to speak there, it says more than I ever could about where the priorities of the healthcare industry lie.
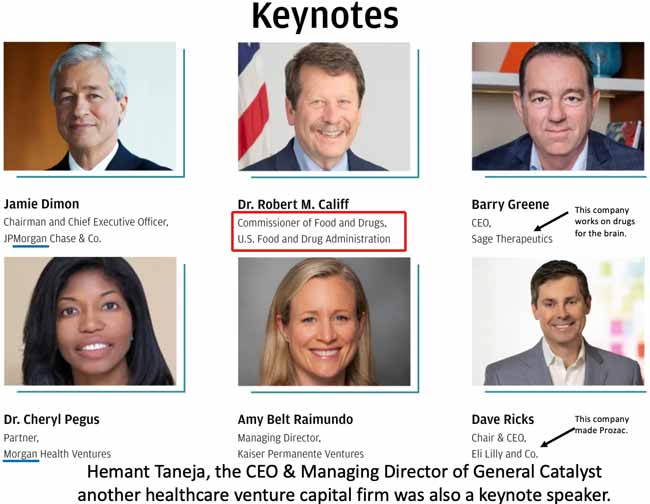
What this lineup essentially says is that the priority of the entire industry is how everyone can make as much money as possible and how interlinked all of this is with the financial sector. That’s not exactly a new revelation, but I rarely see it stated this overtly.
Note: Califf became Biden’s second FDA commissioner on February 15, 2022 (having previously served as Obama’s for 11 months from 2016-2017). At the time, there were serious questions of whether his extensive ties to the pharmaceutical industry made it appropriate for him to lead the agency. To quote Wikipedia:
“Califf worked very closely with pharmaceutical companies at the Duke clinical trials center “convincing them to do large, expensive, and, for Duke, profitable clinical trials.” He was a paid consultant for Merck Sharp & Dohme, Johnson & Johnson, GlaxoSmithKline, AstraZeneca, and Eli Lilly per ProPublica from 2009 to 2013.
The largest consulting payment was $ 87,500 by Johnson & Johnson in 2012, and “most of funds for travel or consulting under $ 5,000”, which has been called “minimal for a physician of his stature”.
From 2013-2014 he was paid a total of $ 52,796; the greatest amount being $ 6,450 from Merck Sharp & Dohme, followed by Amgen, F. Hoffmann-La Roche AG, Janssen Pharmaceutica, Daiichi Sankyo, Sanofi-Aventis, Bristol-Myers Squibb and AstraZeneca.
He was a director of Portola Pharmaceuticals, Inc. from July 2012 to January 26, 2015, an advisor for Proventys, Inc., chairman of the medical advisory board of Regado Biosciences, Inc. and has been a member of that board since June 2, 2009, and a member of the clinical advisory board of Corgentech Inc.
Forbes wrote that his close ties to the drug industry were why he was not nominated for the FDA Commissioner position in 2009. Califf’s ties to the pharmaceutical industry were criticized by the magazine The American Prospect, and Democratic Senators Bernie Sanders and Joe Manchin, who announced their intention to vote against his 2021 renomination [Califf was ultimately confirmed 50-46].”
When Kim sent me this story, she requested for me to review this particular presentation:
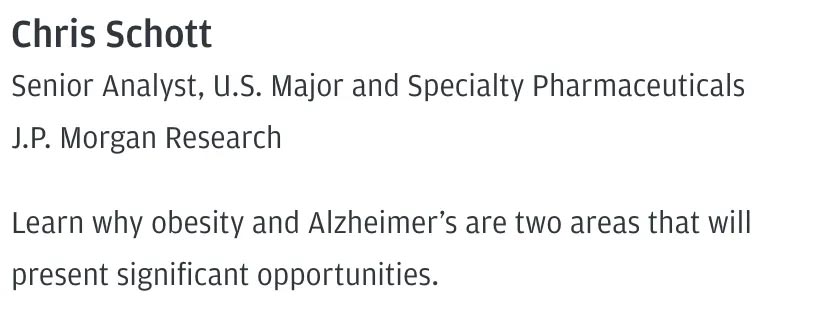
Note: I saved the video (linked above) in case it gets pulled. You may also want to watch it directly on their website (the sound quality is better). The background music they presented in concurrence with this talk (if you see through its euphemisms) highlights how these people see the world and how unconcerned the healthcare industry is with the human costs of their business model.
For this article, I transcribed the analyst’s presentation:
“We’ve seen the pharmaceutical group meaningfully outperform the market in 2022. Now, specifically looking at 2023, I’m most focused on two new therapeutic areas, and these are obesity and Alzheimer’s.
In the obesity market, we have new drugs coming to market, so we see patients effectively not getting diabetes, lower rates of heart attacks, and strokes. So it effectively moves obesity from an aesthetic market to a medical market. We’re forecasting this could be over a 30 billion dollar annual opportunity.”
[Screen flashes to say Obesity — Shifts from an aesthetic market to a medical market $ 30B+ annual opportunity].
“The other market I mention is Alzheimer’s, and this has been by far the largest unmet need in the healthcare industry. I’m encouraged this year we’ll see the first two drugs approved that can actually modify and slow down the rate of Alzheimer’s progression.”
[Screen flashes to say Alzheimer’s — New Treatment Options $ 20-25B annual opportunity].
“When I think of some of the headwinds we could face for this sector in 2023, that could offset some of these positive trends that I mentioned, one that comes to mind is really the sector’s patent cycle, so we’re still facing a number of very large patent expirations as we look out to the end of the decade and I think the investors are increasingly focused on how the industry will manage through those.
What I think about the inflation reduction act and what it means for the pharmaceutical sector as a whole, we view the impact as pretty manageable.”
[Screen flashes to say Inflation Reduction Act impacts: Caps out-of-pocket costs at $ 2,000 for Medicare beneficiaries].
“The bill basically caps out-of-pocket costs for seniors in Medicare at 2000 dollars [this is something people have been fighting for decades]. The more challenging part for the industry is price negotiation. This will be the first time the US government can negotiate drug pricing, and it’s on a relatively limited number of drugs, but it’s something we’ll have to watch closely.
Now going forward and looking out to 2023, the outlook’s still pretty positive in our view. We’ve got core products across the sector performing nicely, we’ve got pipelines continuing to advance and really broaden out, and the sector is not exposed at all to some of the macroeconomic and supply chain volatility that we’re seeing elsewhere in the market.”
There are two main takeaways from this. The first is that the industry (and the investors who enable it) are concerned they may lose some of their ability to price gouge their customers (again, nothing new, but rare to see so overtly admitted). The second is that medications for Alzheimer’s disease and obesity are expected to become two of the biggest franchises in the near future for an industry desperate to develop new drug markets. Kim’s specific reason for sharing all of this was as follows:
“Interesting to also note, FDA Commissioner Califf was keynote speaker on opening day and out of the blue, the FDA granted accelerated approval to the second controversial Biogen Alzheimer drug on Friday [three days before the conference] without an Advisory Committee. How great to be able to announce to the healthcare biotech industry that one of their new drugs was just granted accelerated approval.”
I wish I had more to say, but there isn’t; that, in a nutshell, is the current healthcare industry.
Note: Accelerated approvals for “unmet needs” is a common way the FDA allows pharmaceutical companies to bypass the typical requirements of proving safety and efficacy in order for their drugs to be approved. Kim has witnessed many tragic examples of this during her time on the FDA panel.
Protecting Recurring Sales
Across the globe, the over-the-top censorship and stonewalling of any repurposed (off-patent) pharmaceutical drug for the treatment of COVID-19 opened many people’s eyes to the reality that the pharmaceutical industry (in lockstep with the government) suppresses treatments that threaten the industry’s business model.
Because of the consequences of this stonewalling (e.g., lockdowns predicated on there being no way to treat COVID-19, dangerous hospital protocols instead becoming the standard of care, and disastrous vaccine mandates), it also led them to ask if these monopolistic practices went beyond COVID-19. For example, I repeatedly heard this stated:
“If they went this far for the COVID-19 market does that mean they’ve also done the same with cures for cancer?”
The pharmaceutical business model always aims to have proprietary products that partially improve a chronic condition and must be taken indefinitely (as this ensures the largest amount of sales). If a product is an off-patent pharmaceutical* (so it is no longer possible to make a lot of money selling it) or effectively cures a condition (which quickly destroys its market), that is unacceptable.
Similarly, a non-pharmaceutical treatment must be kept off the market if it does this. The most explicit admission of this situation I’ve seen came from a financial report a few years ago:

“The potential to deliver ‘one shot cures’ is one of the most attractive aspects of gene therapy, genetically-engineered cell therapy and gene editing. However, such treatments offer a very different outlook with regard to recurring revenue versus chronic therapies,” analyst Salveen Richter wrote in the note to clients Tuesday.
“While this proposition carries tremendous value for patients and society, it could represent a challenge for genome medicine developers looking for sustained cash flow.
In the case of infectious diseases such as hepatitis C, curing existing patients also decreases the number of carriers able to transmit the virus to new patients, thus the incident pool also declines … Where an incident pool remains stable (eg, in cancer) the potential for a cure poses less risk to the sustainability of a franchise.”
In a recent series on emotional well-being and coping with trauma, I focused on the treatment options for insomnia because proper sleep is essential for mental health (and healing many other chronic conditions). Presently, while Americans spend over 30 billion dollars annually on sleeping aids (it’s quite a large franchise), most of them don’t work very well.
For example, most sleeping pills sedate you and likewise sedate the brain rather than putting it to sleep — which is a problem because a sedated brain has difficulty performing the vital restorative functions of sleep.
Oddly enough, there is one sleeping medication that is both highly effective in putting the recipient to sleep, and that does not suppress the normal sleep process.
When it was still available, my colleagues found it was a vital component of their treatment plans for chronic illnesses; unfortunately, in the 1990s, it was taken off the market because the media, in a coordinated fashion, whipped up hysteria about it being used for sexual assault, despite no evidence existing to support this (now disproven) claim.
One form of the drug is still possible to obtain (and frequently is very helpful with profound sleeping disorders), but it is challenging to qualify for it. The only way I could interpret those events was that because of how large a market insomnia was, it was unacceptable to have an effective but off-patent treatment for it on the market.
Similarly, suppose you consider the Alzheimer’s examples above because of how much this market is worth. In that case, we have seen billions upon billions be spent to “find a cure” for it (e.g., just for 2021, the NIH spent 2.8 billion), while at the same time, proven treatments for the disease are ignored by the scientific community.
Instead, we have two drugs that cause brain bleeds in 20-40% of the recipients, do not provide any benefit for treating the disease, and yet are so “revolutionary” the FDA commissioner who helped push them through decided to give a keynote address to the entire industry right after approving one of them.
One thing that is often not appreciated about the pharmaceutical industry is that much more money is spent on marketing pharmaceuticals than on developing them. This is because the industry figured out long ago that as long as some case can be made that a product “works,” irrespective of how unsafe or ineffective it is, it can easily be mass marketed to the population.
In turn, because of how much money exists in maintaining this model, many other facets of our society (e.g., doctors, the media, medical journals, and the FDA) have been groomed to support it.
Note: After I completed an article on the causes and treatments of Alzheimer’s disease, multiple readers informed me that they had observed coconut oil noticeably improve the dementia of their ailing parent. I then looked this up and found out there is also scientific evidence to support the observations that were shared with me (e.g., this study).
I share this story because in addition to everyday coconut oil being dramatically cheaper and safer than these “revolutionary” drugs, it also appears to be more effective — which is quite the sad synopsis of our current profit centered healthcare model.
Treating Obesity
The implicit message of the entire conference (and why Kim ultimately sent it to me) was that in the next year, we would start seeing a lot of marketing for treating Alzheimer’s and obesity since these represent the new growth sectors for the industry.
For example, consider this recent article from the Economist, which states that an overwhelming amount of data shows being overweight impairs your chance of financial success and that “it is economically rational for ambitious women to try as hard as possible to be thin.” That is then followed by lamenting how hard it is to lose weight with the presently available options.
This sequence follows the classic American marketing formula — make the viewer experience negative emotions and then present the marketer’s product as a solution to those problems, which I recently argued is a root cause of the emotional distress pervasive throughout modern society.
What I found particularly noteworthy about The Economist’s article was that until recently, stating something like this was taboo as it constituted “fat shaming” because it is understandably hurtful to overweight individuals and thereby creates a variety of harms such as low self-esteem, body dysmorphia, and anorexia.
However, once a profitable product exists to “address” those negative feelings, all of that goes out the window, and those feelings are instead encouraged. So, I can only imagine how much more of this marketing we will see in the near future.
Ozempic
The same corruption in the medical field also exists within the nutritional area. As a result, the processed food industry has convinced much of the nutritional profession that a processed food diet is appropriate for the general population. Because of this widespread ignorance, Americans follow an unhealthy lifestyle, which creates widespread obesity and many other illnesses.
As I discussed here, this, in turn, has led to an endless number of fad diets that don’t really work and torture those trying to follow them (who then inevitably beat themselves up and blame themselves for their failure to lose weight).
I find this a real shame because numerous effective weight loss methods exist (some of which I fully admit I’ve had to use), but like every other competitor to an established medical franchise, they have never been allowed to enter the conversation.
One of the most significant consequences of our flawed nutritional model is the epidemic of diabetes. Most of us know what diabetes is, but unless you work in healthcare (where you will most likely see multiple diabetic patients each day), it is quite challenging to appreciate the magnitude of this problem or how severely it can affect those with it. Similarly, recently the CDC estimated it had cost the United States 327 billion dollars in one year.
While almost everyone recognizes that diet and lifestyle (e.g., basic exercise) can have a massive impact on diabetes, very little focus is given to these areas. Instead, the focus is just on giving more and more pills to lower blood sugar, something which the benefits of doing are often overstated.
One of the medical profession’s hopes for diabetes is that a magic pill will eventually emerge that addresses the disease. While I am seriously doubtful that will ever be the case due to the underlying causes of obesity, many of my colleagues have been quite surprised to see how much semaglutide (branded as Ozempic, Wegovy, and Rybelsus) appears to help diabetics with more severe presentations of the illness.
Many of these benefits result from it reducing the desire to eat, and not surprisingly, weight loss is a common side effect of taking the medication.
Frequently when pharmaceuticals are brought to the market, they are approved for very limited use and then marketed off-label for other uses resulting from the side effects of the drug. Since Ozempic creates that effect, many non-diabetics, in turn, are craving the drug to the point we are facing supply shortages of it.
This situation reminds me of what happened with Viagra in 1999 (discussed in a series about the common patterns seen by Pfizer’s whistleblowers). When Viagra was initially developed, it was created to treat cardiovascular disease (as it dilates blood vessels by increasing nitric oxide production — which is often very good for you).
While its results were promising (and arguably superior to any of the standard treatments), during its clinical trial, Pfizer also noticed that Viagra treated erectile dysfunction and decided to scrap the initially proposed use of the drug to focus on the much larger sexual enhancement market.
Once Viagra hit the market, people were clamoring for the drug (e.g., many urologists told the Pfizer sales rep and later whistleblower that it was the drug they had been waiting their entire career for).
Pfizer instructed all their sales reps not to promote Viagra for anything besides its limited FDA approval (erectile dysfunction in older men with pre-existing circulatory impairment). Still, before long, that was impossible because everyone wanted it (to the point that doctors frequently had to worry about running out of their Viagra samples because staff were stealing it for their personal use).
Since its approval, numerous (sometimes fatal) side effects Pfizer knew about when it brought the drug to market (e.g., heart attacks, strokes, blindness, hearing loss, or melanoma) have been reported, and numerous Viagra lawsuits have been filed against Pfizer.
When Ozempic was first approved in 2017, it was intended to be an adjunctive therapy (along with diet and exercise) for improving blood sugar control in adults with type 2 diabetes. After it was observed that the drug helped with weight loss, a new formulation was made (Wegovy), and in June of 2021, Wegovy was approved for weight loss either overweight adults with a weight-related condition (e.g., diabetes) or those with a BMI of 30 or more.
Shortly after, in May of 2022, a similar drug (Mounjaro) received a similar approval to Ozempic’s 2017 one (as an adjunctive therapy for blood sugar control). Once people realized this drug could help with weight loss, like Viagra, everyone else tried to get these drugs, too, including adults who are not overweight and do not have diabetes. Given that these drugs:
- Have side effects (e.g., nausea, vomiting, diarrhea, abdominal pain, and constipation are commonly reported — additionally, some evidence suggests pancreatic cancer and other severe complications are also associated with this class of drugs).
- The weight loss reverses after stopping the drugs (e.g., one year after stopping semaglutide, participants regained two-thirds of their prior weight loss).
They thus may not represent the best approach for weight loss. Nonetheless, I am sure many normal-weight individuals will pursue them, and both I and colleagues have observed that this is quite detrimental for those normal weight individuals.
Furthermore, unlike in the past, where the FDA to some extent focused on safety, based on Califf’s recent actions (and his long track record of being in bed with the pharmaceutical industry), I suspect that the FDA will do everything they can to allow widespread use of these weight loss drugs.
Note: To illustrate how things had changed at the FDA, in addition to pressuring Pfizer not to market Viagra for off-label uses when it came out in 1998, it also pulled fen-phen in the 1990s because the drug, while effective, created severe complications for its users.
What I find particularly noteworthy about fen-phen is that despite its dangers (and the class action lawsuits that followed) being well known, I periodically heard of cases where desperate healthcare professionals stole it (e.g., from pharmacies) to lose weight.
In short, given the current regulatory environment, I think it is very likely JP Morgan’s prediction will hold, and obesity medications will become a massive drug franchise, especially given that all the currently available ones will require indefinite usage by the consumer. This is a shame because there are much safer and infinitely cheaper ways to accomplish the exact same things these drugs seek to do.
Conclusion
In a recent article on the War in Ukraine, I discussed how, like many others, I have observed that over and over again, once people occupy a certain position of power in the government or corporations, a certain degree of sociopathic thought emerges where they stop caring about the human costs of fulfilling their objectives (such as making more money). Because of this, I have always followed a rule given to me — don’t invest in death.
Friends and relatives throughout their lives have seen countless cases where human suffering or death resulted from investors looking to make a profit without thinking of the human consequences of their actions (e.g., funding mercenaries, investing in defense contractors, or investing in food commodities and thereby making them too expensive for the poor to afford).
While there may be some skepticism to this claim, I, my teachers, who I trust the judgment of, and famous figures throughout history (e.g., Rudolph Steiner) sincerely believed there were real spiritual consequences if an individual left their money with someone who would use it for evil.
For this reason, I’ve lost count of how many investment opportunities I have seen throughout my lifetime (e.g., I discussed the one Biden created with Raytheon in that recent article), I chose not to engage in because the blood that would indirectly be on my hands was not worth a higher rate of return.
I mention this because many encourage investors to focus on investing within their industry because one will typically have a much deeper understanding of that market and which things within it are presently the best bet. Given that the pharmaceutical industry has long been considered one of the best sectors to invest in, and I now know more than I ever wanted to know about the industry, I’ve always thought it was ironic there were the only ones I could not invest in.
Sadly as the recent JP Morgan conference shows, the healthcare industry, and now our regulators as well follow a very different set of ethics.
The tenure of Califf (who is one of the officials most directly responsible for the current vaccine disaster) is enigmatic of the corruption that has seeped into our democracy; Califf’s ties to the industry in just a few years went from being unacceptable to sufficient for multiple tenures as the head of the FDA where Califf can be clearly seen working hand in hand with the pharmaceutical industry.
The best metaphor I can think of for this situation comes from a scene in one of my favorite (satirical) dystopian movies where a sports drink company bought out the entire US government and then had their product replace water throughout the United States. We are at one of those moments in history where everyone needs to work together to reverse the direction we are heading in.
A Note From Dr. Mercola About the Author
A Midwestern Doctor (AMD) is a board-certified physician in the Midwest and a longtime reader of Mercola.com. I appreciate his exceptional insight on a wide range of topics and I’m grateful to share them. I also respect his desire to remain anonymous as he is still on the front lines treating patients. To find more of AMD’s work, be sure to check out The Forgotten Side of Medicine on Substack.
